BACKGROUND:
Subcision is the mainstay of atrophic acne scar treatment but the efficacy and safety of the procedure is controversial.
Various instruments (such as Nokor and conventional needles, cataract blades,and wires) and techniques have been advocated but their effectiveness is indispute.
Moreover, subcision has lost overall popularity given the high risk of needlesticks for surgeons, moderate patient satisfaction,and the possibility of neuro-vascular injuries and also complications such as permanent discoloration.
Blunt Blade Subcision
this novel technique of subcutaneous undermining using a blunt subcision blade seems to be a safe and effective method for atrophic acne scar treatment. The technique is associated with a short recovery time and a low rate of serious complications.In addition, the technique’s simplicity and low cost could make it a suitable first step in the treatment of most cases of atrophic acne scars.
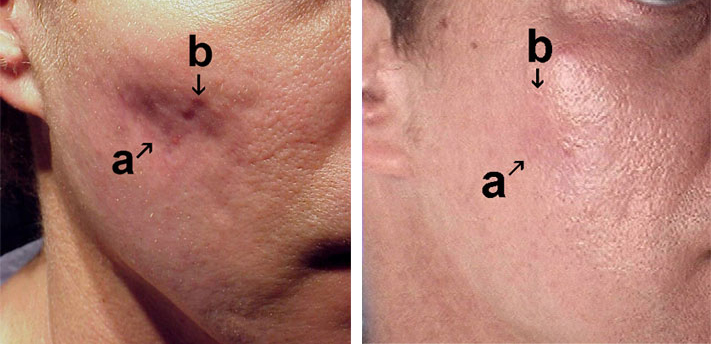
Paper Review: Eighteen patients with bilateral atrophic acne scars considered eligible for subcision were enrolled. Before subcision, a tumescent solution was injected subdermally to anesthetize the treatment area and aid the dissection of the dermal-subcutaneous tissue. Patients underwent treatment using the blunt subcision blade, a long metal blade with gradually narrowing edges, and a rounded blunt tip. Early postoperative complications, overall aesthetic improvement and persistent discoloration, or lumpiness were assessed 7 days after subcision and at a 6-month follow-up visit.
Result
Moderate to marked improvement of atrophic scars was observed in 15 cases (83.3%). Mild to moderate tenderness, periorbital ecchymoses, and swelling were reported by some patients, but resolved completely within 1 week after the procedure. No cases of persistent discoloration or lumpiness were observed at the final visit.